Introduction
Kidney dialysis is the medical process that replaces what normally healthy kidneys do when failing or not performing well enough. The kidney filters harmful chemicals, wastes, and fluid excess in the body’s blood. When the kidneys cannot do this anymore, dialysis has to be done in order to balance the chemicals present in the blood, regulate blood pressure, and work the body as close to normal as possible. What is discussed here includes an explanation of what dialysis is, types available, the most important considerations of a patient, and the most common concerns of a patient undergoing such a life-support treatment.
What is dialysis?
Dialysis refers to the artificial removal of waste and excess fluids from the blood since kidneys are unable to do it under normal conditions. Under normal conditions, the kidneys filter around 120 to 150 quarts of blood daily. This results in 1 to 2 quarts of urine, which serves as a means to dispose of excess salts and other waste. In case the kidneys fail, dialysis is an external filter that performs this vital task.
There are basically two types of kidney dialysis. They are hemodialysis and peritoneal dialysis. Both these techniques have the same ultimate objective but differ in how the procedure is carried out and where it is received.
Types of Dialysis
Hemodialysis
Hemodialysis is the most common of these dialysis procedures, typically done in a hospital or dialysis center; some people also do their dialysis at home. In hemodialysis, blood is filtered outside of the body by a machine referred to as a dialyzer or artificial kidney. This involves inserting a needle into a blood vessel. It will then pump blood to flow through the dialyzer. The blood in this process is cleansed through the machine, thereby allowing the removal of waste products and excess fluids before returning to the body.
Frequency and Duration: Hemodialysis is generally done on three days a week, usually for three to five hours per session, depending on the needs of a patient.
Advantages and disadvantages:
It is very effective in filtering out blood and can be very effective in managing acute cases of kidney failure. Additionally, it requires very frequent visits to a center or a highly advanced hemodialysis setup at the patient’s home, creating potential side effects such as fatigue, low blood pressure, and muscle cramp.
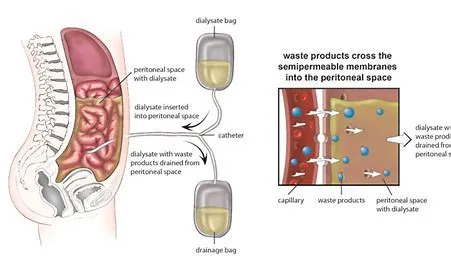
Peritoneal dialysis is more flexible and done at home. Here, instead of the outside machine filtering the blood, a catheter is placed inside the abdomen, and a special fluid named dialysate is allowed inside the abdominal cavity for diffusion to take place as it is filtered by the membrane lining the abdominal wall, termed the peritoneum. The dialysate removes waste products and excess fluids in the blood and then drains and is refilled with fresh solution.
Types of PD:
There are two major types of peritoneal dialysis. CAPD is done manually by patients to exchange fluid four to five times a day, while APD is usually done at night through a machine that automatically fills and drains the abdomen.
Pros and Cons:
PD is more flexible and has fewer dietary restrictions as compared to hemodialysis. So it is suggested for the patients who would like to stay active in their daily routine. But at the same time, it increases the risk of infection like peritonitis. In certain abdominal issues, PD cannot be performed effectively.
Dialysis Considerations
Access to Dialysis and Support Systems
For patients with chronic kidney failure, dialysis can be a lifelong requirement. The frequency of treatments can be physically and emotionally challenging. A patient needs to have access to a dialysis center, means of transportation, and support for the patient to comply and be comfortable.
Patients can also be helped by attending a support group or a dialysis social worker who helps the patient cope with the changes in lifestyle and their emotional well-being.
Diet and Lifestyle Changes

Both types of dialysis require patients to follow certain dietary and fluid restrictions. For instance, a hemodialysis patient is usually limited from taking fluids because excessive fluid results in swelling and blood pressure issues. Foods high in potassium, phosphorus, and sodium should be avoided because these tend to collect in the blood if the kidneys are not functioning well. A renal dietitian can therefore guide these patients on managing their dietary needs while ensuring that they get ample nutrition with their restrictions.
Risk of Complications and Side Effects
Both hemodialysis and peritoneal dialysis have complications. Hemodialysis can cause hypotension, muscle cramps, and infections at the access site. On the other hand, peritoneal dialysis may result in peritonitis, which is an infection of the abdominal cavity. Patients should monitor their symptoms and report any discomfort to their healthcare team. Regular follow-ups and monitoring of blood pressure, electrolyte levels, and access sites are necessary to prevent and manage these complications.
Quality of Life and Mental Health
Dialysis impacts all aspects of life, from work and travel to mental health. Most patients feel tired, anxious, or depressed because of the rigorous regimen and physical demands of dialysis. Counseling, exercise, and association with peers undergoing dialysis help patients cope with the problems and stay optimistic. Others might also seek alternative treatments if possible. For instance, a patient could opt for a kidney transplant if they are eligible and have a willing donor.
Financial and Insurance Considerations
This form of treatment is expensive and chronic, imposing a big financial burden on most patients. Most insurance plans, which include Medicare and Medicaid, pay for dialysis; however, the patient will still face copays and out-of-pocket costs. If the patient is aware of what is covered, the cost of it, and other means of support available, he or she might be in a better place to face the financial stress and devote his or her time and energy toward good health.
Advancements in Dialysis and Future Directions
Dialysis is an area of advancement, as scientists continue to work on how to make dialysis more efficient and accessible. Portable dialysis machines, wearable devices, and regenerative medicine approaches are being developed in an effort to improve patients’ quality of life and reduce the burden of traditional dialysis. Artificial kidney technology innovations aim to eventually replace dialysis with more permanent solutions, such as a bioengineered or implantable artificial kidney.
Conclusion

It has helped millions with a better quality of life from the failing of kidneys by undergoing a life-sustaining treatment: kidney dialysis. It is offered in two significant ways: hemodialysis and peritoneal dialysis, giving patients a variety to choose from that matches their medical needs and personal lives. Dialysis is an art of dedication, with full support and willingness for adjustments in diet, activity, and emotional acceptance of what will be faced through it. Improvements in the field of technology give a ray of hope to betterment in the future, so dialysis is considered a critical area of study and innovation in medical science.



